Thyroid Orbitopathy (Graves’ Disease)
Thyroid orbitopathy is an autoimmune inflammatory disorder of uncertain etiology that affects the tissues of the orbit (i.e. eyelids, extraocular muscles and other soft tissues surrounding the eyes). Patients with this disorder often have an associated thyroid abnormality which may manifest either before, during or after the orbital signs and symptoms. A small percentage of patients may have eyelid and orbital manifestations without developing a thyroid abnormality.
Thyroid orbitopathy can develop and affect patients with varying degrees of severity. The disease may begin suddenly and progress rapidly over days to weeks, or can start insidiously and progress gradually over a long period of time. The majority of patients have mild inflammation, the most common signs and symptoms of which are retraction of the upper and/or lower eyelids and bulging of the eyes. In cases with more moderate inflammation, patients may also have varying degrees of double vision and eyelid swelling as well as visible redness of the lids and eyes. A small percentage of patients with thyroid eye disease develop severe inflammation, which can result in compression of the optic nerve and permanent vision loss. In most cases, the inflammatory process is self-limited and runs a course lasting 6 months to a few years before subsiding. After the inflammatory phase of the disease subsides, scarring of eyelid and orbital tissues may result in the persistence of eyelid retraction, proptosis and double vision.
During the inflammatory phase of the disease, patients are usually evaluated on an interval basis to monitor progression of the disease and managed with measures to reduce ocular symptoms. Care is coordinated with the patient’s endocrinologist, who will manage concurrent thyroid abnormalities. Once the inflammatory phase of the disease has subsided, patients with eyelid abnormalities, double-vision or proptosis may be eligible for surgical correction to improve their function and appearance. It is important to note that cigarette smoking has been associated with worsening thyroid orbitopathy, therefore cessation of smoking is universally recommended in thyroid patients.
Orbital Tumors and Trauma
The orbit is a small, compact and complex structure. Oculofacial surgeons specialize in the in this area of the face and have the extra training required to care for these problems in children and adults.
In both children and adults, a variety of tumors can occur in the eye socket. Some grow slowly, and go unnoticed while others can grow rapidly; impairing vision and causing even greater problems. CT scans and MRI’s are the best method for detecting and differentiating these lesions prior to having surgery. Once the location and the general characteristics of the lesion have been identified, a treatment plan can be created. In some instances your orbital surgeon can treat these tumors on their own, often as an outpatient. On the other hand, aggressive tumors may require the help of other surgical specialist and in patient hospital treatment.
In the United States, injuries to the eyes and eye socket are unfortunately common place. Eyelid laceration, tear drain injuries, bleeding within and bruising around the eye, and fractures of the bones of the eye socket can all occur. These injuries often occur from sporting activities, car accidents, or fist fights. Trauma to the orbit and eye area most often results in bruising followed by fractures of the orbital bone blowing out into the surrounding sinus. Fractures causing double vision or large fractures into the sinus should typically be repaired in a timely fashion. In cases when this is not possible, late repairs, despite being more difficult, can still be performed.
Sometimes trauma is severe enough to irreparably injure the eye. Diseased eyes that are blind, painful and disfiguring can be the removed when the eye can not be salvaged. Reconstruction of the eye socket to prepare it for a prosthetic eye typically leads to a very pleasing result. Eye sockets that have already had the eye removed require regular examinations and may need further reconstruction.
Lacrimal Surgery
The tear film on the surface of the eye is a critical component of maintaining vision. Tears nourish and lubricate the surface of the eye and wash away debris. A smooth, balanced tear film also allows light to enter the eye in an optimal fashion. If there is a disturbance of the tear film, patients will often experience tearing, burning, irritation and most importantly blurred vision. Patients who experience tearing may have a problem with tear production or tear drainage.
Problems with tear production may be related to aging and menopause, or may be the result of inflammatory conditions such as rosacea, rheumatoid arthritis and Sjogrens disease. As tear production diminishes, the surface of the eye starts to dry out. The body senses that the eye is dry and irritated and signals the main tear gland to flush the eye. As a result, the dry eye paradoxically tears. Patients with dry eyes note intermittent tearing of the eyes during activities such as reading, driving, watching TV or a computer screen, or going outside on a windy day. These all cause the eye to dry out because it blinks less during these activities. The treatments for dry eyes include 1) replacing tears with artificial lubricants which can be bought over the counter, 2) medications like Restasis that decrease inflammation in tear glands and encourages natural tear production, and 3) plugging of the tear drain.
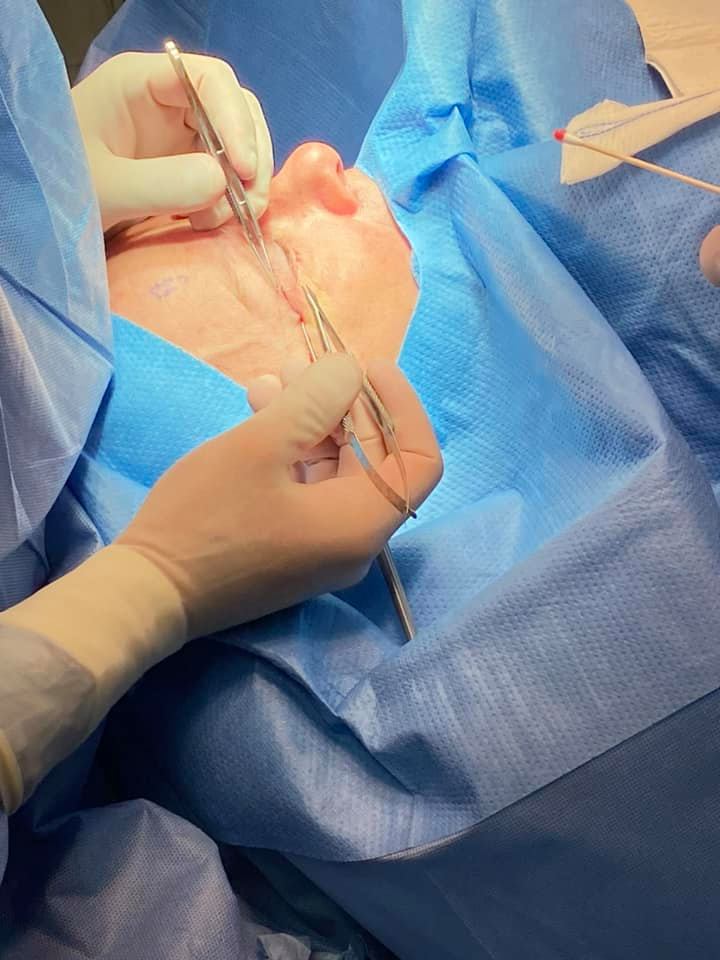
If the tear passageways become blocked, tears cannot drain properly and may overflow from the eyelids onto the face. Additional symptoms may include blurred vision, mucous discharge, eye irritation, and painful swelling in the inner corner of the eyelids. This obstruction may result from aging, trauma, inflammatory conditions, medications and tumors. In mild cases, dilation and irrigation and/or stenting of the lacrimal passageways may improve the obstruction. In more severe cases, surgical intervention to bypass the tear duct obstruction (dacryocystorhinostomy or DCR surgery) may be recommended. A DCR is performed by creating a new tear passageway from the lacrimal sac to the nose, bypassing the obstruction. This is usually performed as an outpatient procedure. Patients usually have some bruising and swelling on the side of the nose that subsides in one to two weeks. In general, surgery has a greater than 95% success rate and most patients experience a resolution of their tearing and discharge problems.